Salt // four
And in a blink of an eye, Salt is four! The last 12 months really have flown by, which is a strange feeling given the pandemic simultaneously feels like it’s lasted forever. We almost feel grown up now, fully established and excited about where we are, as well as what’s still to come. It’s clearly not been the easiest of years for anyone, but our team and our clients have continued to inspire us and we are incredibly proud of what we’ve achieved in the last 12 months.
This time last year we thought we were heading back towards ‘normal’ life. This year, hopefully, we actually are. While it’s been one of our best years so far in terms of the team, the work and what we have achieved, we are really hoping we can top it next year with a bit more interaction and freedom to spend time with people. We’ve missed that a lot, and we can’t wait to get back to it. Bring it on!
Lewy Body Dementia Awareness Week - a personal story
This week is Lewy Body Dementia Awareness Week[1]. Despite my Dad having had LBD I had no idea the awareness week existed. I guess that’s why we need to raise awareness. Lewy Body Dementia, for those of you who don’t know, is the second biggest cause of dementia in the UK and is basically the delightful double whammy of Alzheimer’s disease and Parkinson’s disease rolled into one.
An article[2] on my university alumnae page about LBD Awareness Week drew my attention – a personal essay by author Jane Sigaloff about her Father’s journey with LBD. The essay calls for people to share their own stories with the aim of raising awareness and support those who are currently going through it. Like with so many conditions, change starts with awareness, so, with the approval of my Mum and sister, I am sharing my story too.
On reading Jane’s essay I was immediately struck by the similarities between her Dad’s story and mine. First it was the spooky coincidences – her Dad was also called Peter, also diagnosed in 2015, also died in 2019 and also at the age of 76. That was weird, but reading on there were so many other parallels in the way she described her Dad’s journey with LBD that it really struck a chord. We were never given a lot of information and certainly whenever we asked what we could expect we were told there was no set path and therefore we had nothing to support or prepare us for how things would evolve over the coming years. That is certainly something that needs to change.
In recent months I have found myself thinking about Dad a lot more. I’m not exactly sure why, maybe it’s just how grief has panned out for me, maybe it’s because of the pandemic and endless lockdowns, maybe it’s because I have recently moved house and feel like I want him to be a part of a home that I know he will never visit. Almost immediately after Dad died I found it hard to remember what he was like when he was ill. Like I immediately erased those few years and was finally able to remember him when he was well, which I struggled to do in the last years of his life. Jane’s article reminded me of so many things that I had already forgotten.
Things started a good few years before he was diagnosed. There were silly things, like not being able to remember where he’d put his cup of coffee, words stubbornly stuck on the tip of his tongue, or accidentally calling Kidderminster, our nearest big town, ‘Swindon’, the town we had lived near to 30 years previously. Things we all do sometimes, but it became a regular occurrence. On these occasions he would give a little sideways glance, curl the corners of his mouth up slightly and acknowledge with humour that he was ‘having a bit of a senior moment’. These smiles were lovely to see as his facial expressions had started to become a lot less animated, even a little empty and vacant at times. Always a keen walker, he started to become a bit flat footed, not so steady on his feet. Then came the little things that we couldn’t quite put our finger on. Tiny, insignificant things that weren’t wrong but just not quite his usual behaviour. Like he was ever so slightly different to how he had always been.
Then the night-time wandering started. As with so many men his age he had been bothered by his prostate for several years, but his waking gradually became more challenging. He would wake up disorientated, opening the curtains or wandering down the landing in search of the bathroom that had been in exactly the same place for the last 30 years. On holiday once, a cruise, he opened the cabin door instead of the bathroom door and was left wandering around the corridors in his pyjamas in the middle of the night trying to find his way back.
He didn’t worry too much about any of these things, he took them to be nothing more than normal ageing. But we knew it was more than that. I had run campaigns for dementia brands in the past and had obviously taken to Google to try and piece together these symptoms, so I suggested that Mum speak to their GP about it to see if there was any sort of early assessment and intervention we could try. While the GP listened and made notes, all they suggested was to call him in for a general health check. Clean bill of health later, we were no further down the line and it felt like we were just waiting for the inevitable decline before any action could be taken. We were totally helpless.
There was one really defining moment. Away on another cruise (these extravagant holidays were severely lacking in my childhood!), my parents were sitting up on deck after dinner, watching the sea go by and drinking a G&T. Mum said ‘well, I guess we should think about heading back to the cabin’ at which point Dad appeared outraged. ‘You can’t come back with me!’ he announced, shocked at her proposition. A long debate ensued, during which it became apparent that Dad didn’t realise that Mum was his wife. His wife of over 40 years in fact. Now the general advice for dementia is to go along with the delusions, because to the person experiencing it they are totally real. It’s like trying to argue with someone that the sky is in fact green when they can clearly see it is blue. Easier said than done when you are in the middle of the Indian Ocean and being faced with your husband having a psychotic episode and being refused access to your bed for the night. Eventually, after showing Dad her passport, he conceded to let her in but was still very unhappy about it. I can’t begin to imagine how it made Mum feel – anxious, scared, vulnerable, alone, and much more I’m sure. She didn’t even tell anyone until they got home two weeks later.
Totally out of nowhere, he had suddenly mistaken his wife for an identical imposter. That might seem like a random thing to be confused about, but it was actually the key to his diagnosis. This seemingly preposterous and highly specific delusion is often listed as a common symptom of LBD, and so helped us re-start the conversation with his GP and reach a diagnosis.
But it certainly wasn’t straightforward from there. There are no approved treatments for LBD, the best you can do is try Alzheimer’s and/or Parkinson’s medication and see what works. The dual nature of LBD means that all too often you end up having to make a choice between body and mind, as the treatments that help one will often worsen the other. As things progressed he needed a stick to walk. Then two sticks, then a frame, then a wheelchair. He slept less and less at night and more and more in the day. His independence drifted away from him, along with his ability to judge time, space and reason. He became agitated, stubborn, obsessed with making plans (okay, so he was always a little bit like that, but this was a whole different level). We had to run through detailed plans for everything – even a trip to the supermarket – several times over in the days leading up to it. It got to the point where we stopped telling him about things in advance for fear of him becoming obsessed with planning. He became unsteady on his feet, his left foot in particular being reluctant to lift off the ground. He fell a few times, nothing major, but enough to frighten himself (and us).
After receiving his diagnosis he was told he would have to re-sit his driving test if he wanted to keep his licence. We all knew his driving hadn’t been great for a while, a big thing for Dad as it had always been such a big part of his life. From buying a de-commissioned black cab with his mates in the 60s and driving it across Europe, to family days out in the 80s ‘going for a drive’, to his retirement job delivering new cars all across the country for the local Vauxhall garage, driving was always something that made him happy. While we all hoped he would decide not to sit it, he of course was adamant. He sat it, and he failed. He spent months complaining about how the examiner had got this wrong and that wrong and about how he was going to appeal the decision, but over time he got used to being chauffeured around by Mum and I think also lost the desire for it as his body and mind continued to decline.
His walking became incredibly slow and laboured. His behaviour became increasingly difficult, even aggressive. My Dad was certainly not an aggressive man, in fact at his funeral I lost count of the number of people who described him as a gentle man, with a cheeky sparkle in his eye. So to see him shouting, calling people names (especially my Mum, his primary carer) was hard. He had a string of UTIs that each marked a significant decline in his mental and physical health, every time dropping him a notch further towards incapacitation. He became incredibly hard to manage, refusing to take his medication, spitting it out, often taking an hour to be persuaded to take one tablet, which clearly requires the patience of a saint (in the form of my Mum). Mum, by this time, was doing everything for him. She would be awake all night as he tossed and turned, and even when he slept she found it hard to do the same for fear of what might happen if she wasn’t watching him. She would spend the whole day looking after him and dealing with however he expressed himself that day. She had to make sure he took his medication, he ate a decent meal, he drank fluids. She had to lift him up every time he stood, support him every time he walked, help him as he got in and out of the car. The strain on the primary carer, mentally, physically and emotionally, is immense.
He also started experiencing more and more hallucinations and delusions. He would often talk to people who weren’t there, having full conversations. Or imagine there were dogs or spiders in the bedroom at night. One common one was that the entire Welsh rugby team were hanging out in the bathroom. Almost like dreams, it fascinates me to think about why he produced these particular things to obsess about, what was going on in his mind that popped these particular realities in there for him? He also moved backwards through time, initially thinking he was back at work and talking about invoices and having to do things on the computer. Then he went further back, talking often about someone he worked with briefly many years ago. Again, I have no idea why this particular colleague became such a fixture.
One day, in spring 2019, he fell while in the waiting room at the local GP surgery. Just a little trip, nothing significant. Three of the staff came to help, but they couldn’t lift him. He had so little control over his body that he was like a dead weight, so they had to call an ambulance to lift him up off the floor and into an examination room. Everything seemed to be fine, he was talking, aware of what had happened, and even a little embarrassed at all the fuss. After a little while they helped him out to the car and Mum drove him home. She managed to get him as far as the dining chair by the door while she made dinner, then to his chair in the living room after they ate, but from there he refused to move. He fell asleep and in the end she had no choice but to leave him there for the night. Next morning she called the GP to explain what had happened, and they sent another ambulance out. This time he was taken to hospital and that night in the chair was the last he spent at home.
He had an infection, and like all the UTIs beforehand it knocked him badly. Despite his initial lucidity immediately after the fall, within a few hours it was a different story. That was the last day he walked, last time he spoke any sense. He spent a week in hospital and was then discharged to a care home for two weeks’ rehab before coming home. In those two weeks he developed another infection, had another stint in hospital and was then discharged, bedridden, back to the care home. I’m not sure if we ever said out loud to each other that he was never coming back home, but I think we knew it. He didn’t really know who we were anymore. We would visit him and sometimes he would show vague recognition, sometimes he would barely acknowledge we were there. Only once in the 8 months he spent in the home did he call my Mum by her name. But, he was content. He seemed calmer there, more compliant certainly for the team of carers than he was for Mum at home. Less agitated, less aggressive, more at peace with where he was and who he was. Maybe he did recognise us because he always made more of an effort for the less regular visitors! His sister, a neighbour, and old friend, he always seemed more alert and aware when they visited, like he was playing host and had to make an effort.
He communicated very little by now. He would mumble so quietly you could barely hear him, and what he did say never made any sense. Music is known to trigger good responses in people suffering from dementia and Dad was no different, while he could barely speak, he would sometimes sing along to music that was playing in the background, especially good old 60s rock. The last time I saw him my kids had made him birthday cupcakes. They took them in, so excited to give them to him. We put one in his hand and he scoffed the lot, I think I even saw a flicker of a smile as he licked his lips. That was a good day.
On 17th December 2019 we got the call. He woke up in the morning but was barely awake, they knew straight away that things weren’t good. Mum went over but arrived just a little too late. My sister and I didn’t really get to say goodbye. Although, as is almost always the case with dementia, he had really gone long before. There never is a chance to say goodbye as you can never define the moment when they are ‘gone’. It happened over a number of years, in Dad’s case fairly swiftly, and there is no one moment you can look back on as being your last. There are memories, moments, conversations and of course a connection that will never be gone.
While the loss of a parent is never something to be thankful for, we could take solace in the fact that he was no longer trapped, no longer suffering, and no long a shell of his former self. That’s almost what it was like by the end, a shell with no way of knowing what, if anything, was going on inside. I am comforted to know that the day before he died was a good one. He was in high spirits and had been bright and relatively chatty with Mum, my niece and his carers. When he was getting ready for bed he started singing ‘Let It Be’, by the Beatles. So his carer looked it up on YouTube and played it for him, and he sang along to every word. I like to think he fell asleep happy, and maybe ‘Let It Be’ was a final message to those of us he left behind.
These days, we have plenty to remember him by, and to make us smile. He pops up in unexpected places too, like finding that my new garden is full of forget-me-nots, the flower of dementia. My Mum and my sister have taken some back to plant in their gardens at home.
Why am I sharing all of this? Like I said, change starts with awareness. Awareness of what this condition is, what we can do and how we can help. There is still so much stigma around dementia, which needs to change. Access to good care, and residential care especially, desperately needs to improve. There is so little known about LBD, and that certainly need to change. We need to start exploring LBD – what are the causes, the triggers, are there any ways we can slow or prevent it, can we develop treatments for it, even a cure one day. Why not? But until there is enough awareness and conviction to change, nothing will happen.
LBD is hard. And it’s amazing to believe that it is so common and yet, for some reason, still so unknown. If this can help spread a little more awareness, and in turn help lead to more support, recognition, funding and research, then it is worth sharing. I hope Dad would agree.
I am running a half-marathon this Sunday in memory of my Dad, and if anyone feels able to contribute you can find the link at the bottom of this page3.
Thank you for listening.
1. https://www.lewybody.org/lewy-body-dementia-awareness-week-dotty-days-6-12-june-2021/
One year on
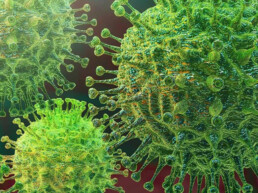
A year ago today I was battling a nasty respiratory virus that may or may not have been COVID-19. I still don’t know. Reading this post again, it is amazing how much has changed in the last year. How much we have learned, how much society has adapted, how far medicine and healthcare have advanced. It’s astounding that we have all been adapting our daily lives for a year now, never quite sure when the end will come.
We have missed so much – people, events, journeys, adventure. But as a society we have discovered so much too, forced to adapt how we do things and accelerate change much quicker than we otherwise would have. While we’d clearly be better off if this pandemic had never happened, we can at least be proud of the
accelerated progress we have achieved in areas that have been slow to change, like virtual healthcare, flexible working and medical R&D. The development, approval and roll out of the vaccines have been nothing short of a human miracle.
Last year’s post may seem naïve now, but it’s also a sign of how far we’ve come. Hooray for vaccines, hooray for gradual easing of lockdown, and here’s hoping we can keep this virus in check.
Here’s to meeting with friends, holidays, haircuts and hugs. Enjoy 🙂
Have I had coronavirus?
Will the planet thank us for COVID-19?
It’s approaching the time of year where we offset Salt’s carbon emissions. Being a virtual agency our footprint has never been huge, but this year I am obviously expecting it to be lower than usual. The reduction in travel globally has clearly been good news for the planet, but it got me thinking about the wider environmental impact of the COVID-19 pandemic.
The early days of lockdown brought much needed good news of smog-free skies, wildlife running free in urban areas, the canals of Venice being the clearest they have been in 60 years, a reduction in intensive fishing and many other reported silver linings. They brought hope that our planet was getting a chance to come up for air, take a deep breath and go about its business without the incessant interference of human beings. It was heartening to believe that the pandemic, while clearly a disaster of great proportions for humanity, could become a trigger for more environmentally conscious behaviour after seeing what the world can do when the human race slows down for just a few months. Perhaps it could trigger the green movement to become more acutely urgent and motivating, encouraging everyone to treat the world with a little more care and consideration. I think most of us were left with the belief that at least the pandemic has been good for the environment.
But is it panning out this way? As the pandemic has progressed the environmental impact has already begun to shift. While a reduction in travel has been beneficial, now that restrictions are easing travel is rapidly creeping back up. Beyond travel, single-use plastic use has dramatically increased with gloves, masks, plastic screens and PPE, we are using more cleaning products (from harsh bleaches and household cleaners to laundry detergent and handwash), and of course with everyone at home domestic energy use is higher than usual. Illegal deforestation in the Amazon has been able to continue unchecked, and it’s likely that similar habitats around the world have suffered due to the lack of patrolling. Even areas where great progress had been made, like reusable coffee cups, have had to revert to single-use alternatives. For how long we can’t be sure, but possibly long enough to forget the habit of taking your own cup and re-learn the habit of using a disposable one.
It is well understood that behaviour change is likely to be more successful if the intervention is aligned to a moment when the existing behaviour is disrupted. In other words, being forced to break one habit is the perfect time to nudge us into establishing a new one. The average habit takes about 10 weeks to form, which makes lockdown the perfect opportunity for governments to intervene and encourage people to form new, lower carbon habits and prevent a default return to how things have always been. What we appear to be seeing, however, are economic recovery drives to get industries like construction and fossil fuels moving faster than ever, with payouts and the relaxing of regulations and royalties. To quote Tom Heap from BBC Radio 4’s Costing the Earth, we appear to be ‘taking the green handcuffs off business’.
The pandemic has clearly taken focus from the momentum the environmental movement was gaining. COVID-19 has naturally had to come first, but we need to make sure we don’t forget where we got to and can continue to move forward rather than taking a step back and starting again. It feels such a shame if we can’t at least grasp the opportunity to take stock and change our behaviour for the better. After all, our planet will be here a lot longer than we will.
But that’s exactly the problem. Environmental impact is a long-term issue, not urgent enough for us to change our behaviour now for the promise of a better future in the long-term. COVID-19 has given us the unique opportunity to see with our own eyes the impact our actions have on the planet, almost a brief window into a parallel world where the environment is higher up the agenda. It would be great if this realisation developed into a positive legacy of the pandemic, so at least some good comes of it.
“…As we recover, the decisions we make today will either lay the foundation for sound, sustainable and inclusive growth, or lock-in polluting emissions for decades, and in doing so make our society and the planet more vulnerable.”
Delivered by Justin Addison, Second Secretary at the UK Delegation to the OSCE, at the virtual OSCE Economic and Environmental Committee Meeting on 3 June 2020.
As we come out of lockdown (for now at least), maybe we should all consider which new habits we can keep, to be more conscious and mindful of our impact on the environment. Let’s celebrate re-gaining our freedom and being able to see friends and loved ones, but let’s not default to how things were just because that’s how they have always been.
A change in routine is a key opportunity to create lasting behaviour changing by forming new, long-lasting habits. Let’s make sure we take it.
#covid19impact hashtag#environment hashtag#environmentalimpact hashtag#coronavirusimpact
Have I had coronavirus?
Notes from my sick bed
The simple answer is, I don’t know. The guidance to self-isolate if you are showing symptoms came at the same time as the guidance to only test people who are hospitalised. I have had a persistent dry cough, difficulties breathing and a mild fever. But I will never know whether it is COVID-19.
I don’t know why testing is being restricted to hopsitalised patients, but I suspect it due to limitations on testing capacity. This is currently being ‘ramped up’ [1], and if my theory is correct then it is absolutely right to reserve the limited resources for those who need them most. But you can’t treat COVID-19 anyway, so what’s the point of testing for it?
Well, what are the implications of people self-isolating and not knowing whether or not they have been infected with COVID-19?
My symptoms started on Monday 9th March, with a very sore throat followed by a cough and a tight chest. The sore throat was short-lived, but as the cough got worse my breathing difficulties followed. By Wednesday evening I was struggling. I had very little energy, even walking around the house felt like a lot of effort, and my blood oxygen level was only 90%. Being an asthmatic, a chest infection like this over winter isn’t unusual for me, so I was working on the assumption it was fairly routine. In usual circumstances, by this stage I would go to see my GP to have my breathing assessed and appropriate treatment given.
However, as I was about to do this, the guidance came for everyone with symptoms to self-isolate. I was stuck, I needed medical assessment but I wasn’t allowed to go anywhere. The lack of testing to either confirm or deny my diagnosis left me at risk. I called 111 and was escalated through the call centre to a paramedic, GP and then her supervisor as to what action should be taken. The end result was that I was issued antibiotics and oral steroids to boost my usual inhalers (that I had already doubled the dose of). Neither of these would be effective against COVD-19.
By Saturday afternoon, I was starting to feel a little better. This is most likely to be a response to meds, which would indicate I was negative to COVID-19. Or maybe it was COVID-19 and I was over the worst of it – the NHS guidance suggests you should start feeling better with 7 days[2], and Saturday was day 6 for me. My improvement has done nothing to confirm or deny a COVID-19 diagnosis.
Why does it matter that I don’t know?
- If it was COVID-19 then everyone I have been in recent contact with should have been self-isolating too. Because it hasn’t been confirmed this hasn’t happened, and these people could be walking around spreading the virus to anyone around them. This includes the elderly, vulnerable, or those in high risk groups, which is why isolation is so important in the first place.
- If I have had it, it would mean I could help others as they isolate. I have no doubt that isolation guidance is going to get a lot more stringent, and if I have already been exposed I could be one of few people able to get out and about to help friends, family, the vulnerable and the wider community A small number of people have been be re-infected [3], but that is by far the minority. The early-exposed will be those we come to rely on as movement of people becomes even more restricted.
- If we don’t test everyone with symptoms, we can’t know how many people are infected and therefore don’t know where we site on the infection curve. Sure, we can estimate it by extrapolating the data back, but that is an estimate and may lead to incorrect strategies being put in place if we falsely estimate the stage we are in.
- People who need medical attention are unable to seek it unless it becomes so ill that they need to be hospitalised. If a hospital is the only place they can be assessed, this puts added strain on the hospital system, which we know is already under huge pressure and drastic measures are being taken to plan for worse to come. Early assessment in conditions like asthma is designed to prevent exactly this – people ending up in hospital who could otherwise have managed their symptoms to prevent escalation. That is bad for a system under pressure, and bad for people who have to endure life-threatening symptoms for a disease we should, by and large, be able to manage through early intervention. At the time of writing there is no specific guidance for those with COVID-19 symptoms and underlying asthma [4]. I am sure parallels could be drawn to other conditions on the at-risk list.
In my view, we have to hope for wider testing of those with symptoms so we can overcome these issues. That is easy to say, and there will be a million priorities fighting for time, resource and budget among this crisis. As for me, I am getting better, my isolation ends tomorrow and hope I have had it. If I haven’t, then surely it is still to come.
I can’t even begin to comprehend the impact this is going to have on the world, a true human tragedy. Stay safe everyone.
PS. Random coronavirus fact. Corona means “crown,” and the viruses are named for the proteins on the outside of the viruses that look like crowns. [5]
1. https://www.bbc.co.uk/news/health-51814874
2. https://www.nhs.uk/conditions/coronavirus-covid-19/self-isolation-advice/
4. https://www.asthma.org.uk/advice/triggers/coronavirus-covid-19/
5. https://www.healthline.com/health/coronavirus-incubation-period#other-coronaviruses
I am not a vegan
I became a vegetarian back in the 1980s. In those days it was far from common, and it was hard to find vegetarian food when I was away from home. My friends’ parents didn’t know how to deal with it, and my Dad thought I was some kind of hippy weirdo who would get over it by the time I hit my teenage years. 30 years on, I am still vegetarian. But recently, and entirely out of my control, I am becoming more and more vegan. I am perfectly happy being vegetarian, and although I have reduced my dairy consumption, I have absolutely no plans to become vegan. But society disagrees. Since the recent rise of the vegan movement, vegetarians have been side-lined. It’s great that so many people are turning to veganism, but I don’t see why it should be assumed that I automatically want to join them. All of a sudden, most pubs and restaurants have few if any vegetarian options, instead proudly announcing their new vegan credentials and expecting me to be delighted.
There’s no doubt veganism is on the rise. The number of vegans in Britain quadrupled between 2014 and 2018, now standing at 1.16% of the population[1]. In contrast, 14% of the UK population is vegetarian[2]. In addition to these two figures, 21% of UK consumers currently identify as being ‘flexitarian’ – eating a largely plant-based diet that is supplemented occasionally with meat. Looking at these statistics, why is it that vegetarian dishes on the menu have been replaced with vegan ones? There are still more than 12 times as many vegetarians as vegans, so why should vegetarian options be struck off? Would it not be more representative of current dietary choices to reduce the number of meat-containing meals instead of sacrificing the vegetarian ones? Shouldn’t we be providing a greater range of options that reflect the spectrum of diet choices across the population?
There is a wild assumption that vegetarians will be happy to be vegan. Why is that so? I have chosen to cut meat and fish from my diet, but I don’t exclude eggs or dairy. The reaction to rising veganism has been to lump two customer groups together and assume everyone will be happy, rather than to understand the needs of each and catering (literally) to them accordingly. I’m about as delighted about being pushed into veganism as a meat eater who is suddenly told they have to be vegetarian.
I have experienced some hilarious assumptions as a vegetarian. Like the time I got a slightly smaller Mars bar than the non-vegetarians on an in-flight meal. Or last month when my meal at a Sofitel in France was a bowl of vegetables that looked identical to something I could have microwaved myself, straight from the freezer. For the bargain price of €22.
My point is that we shouldn’t be lumping people into buckets and going with the easy option. (Even when looking for stats on vegetarianism for this post the search results were largely about veganism, despite it not being in my search terms.) Instead we should be recognising different customer groups and their needs, and providing choices that reflect that. And also, I really love cheese…
- https://www.vegansociety.com/news/media/statistics
- https://www.comparethemarket.com/car-insurance/content/cars-against-humanity/
- https://www.theguardian.com/business/2018/nov/01/third-of-britons-have-stopped-or-reduced-meat-eating-vegan-vegetarian-report
Salt // two
The last 12 months have been amazing.
When we turned one we reflected on why we started Salt, saying ‘We wanted to feel free to enjoy what we do, put our experience to good use, make a difference, and to simplify and streamline the way we work so we can offer people more.’ We had certainly done some of that in year one, but looking back now on year two, we have done a whole lot more. Our second year has seen us doing even more exciting things, expand our client base, work with a growing team of wonderful associates and partners, travel more than we ever expected, deliver a global campaign and embark on a new EU launch. Aside from that we’ve built escape rooms, life-sized board games, VR experiences, art installations in Lyon’s Museum of Contemporary Art, created a hair salon on a congress booth, turned scientific data into art…and made sure we’ve always had time to enjoy it along the way.
We have continued to meet and be inspired by amazing people, grasp amazing opportunities and get far too carried away with our ideas on many an occasion. We have an excellent team of people we rely on to make Salt a reality, and we thank each and every one of them for helping us to complete our second year as a thriving business, doing work that really matters. Our clients have given us feedback that has made us blush and even cry (in a good way!), and we have seen the impact of some of our work out in the real world. That’s really what we want to achieve – creating positive change in people’s lives.
Please can we have more years like this one? We have honestly loved every minute.
How can this be okay?
Salt is now in its second year, and things are going well. We’re getting busier by the day, with lots of new clients coming on board and existing work expanding into new areas. So how come our cash surplus is disappearing before our eyes, and our bank balance is fast approaching zero?
It’s no surprise that cashflow is one of the biggest challenges for any business, especially a start-up. We started our business with nothing – no clients, no funding, no loans and no overdrafts – so we knew it would take a while to get things going. Once that started happening, thankfully only a few months in, we were able to play catch up and keep ourselves afloat. Small and midsized companies generally seem to understand and appreciate this situation, and manage their finances accordingly to honour their payment commitments to the letter. Unfortunately, we are seeing more and more cases where the larger, global organisations do not.
Large corporations, with annual revenues over $30bn, appear to have a systematic culture of late payment, and I am yet to work out why. Is it because those extra weeks keeping hold of your budget gives them an advantage? Is it just laziness or inefficiency? Is it that they simply don’t appreciate that withholding funds can put small businesses at risk? Or is it a power trip – they know they can get away with it? Who knows. An awful lot of time and energy is put into negotiating a contract, yet it seems to mean very little when one side can break it at will. Somehow dealings between two businesses don’t need to conform to the same principles we might put on a person-to-person interaction, and it makes it okay to break the rules without explanation, apology, accountability or consequences.
Being business to business can make the conversation, decisions, actions and principles less human, so it suddenly becomes okay not to pay people what you owe, blaming the system and the rules rather than seeing that it is clearly unfair and taking responsibility. I see no reason why commitments should be any less important in the commercial world than they are in the personal world, particularly if the relationship is valued. And that’s always a sticking point – the clients we work directly with do value the relationship, as do we, so inevitably it is the small businesses that have to compromise in order to maintain it. It is the small business that is asked to start work without a PO, deliver work with no idea of when they might be paid, and take on all the financial risk and burden associated with doing a good piece of work in the spirit of ‘partnership’. It’s totally out of balance, and plays on people’s good nature, willingness to do good work and not wanting to be the one who prevents something from happening. And clearly, a small business is never going to sue a global corporate entity for not fulfilling their contractual obligation to pay on time, so all is well.
Or is it? Is it okay for small business to bankroll gigantic corporate entities? Should we be taking all the risk, uncertainty and cost of bridging the gap? Should we accept that so many good small businesses go under because of these sorts of practices?
We operate our business fairly. That means we pay our associates and partners on time, and we respect their need to run a business as much as we do our own. Because for us, money committed is just that – a commitment, a promise, and fair remuneration for good work. Working this way leaves us exposed in the middle – honouring our payment commitments without being able to rely on the same for our income. Some people may say it’s naïve, but we feel good business is all about being true to your principles. Agencies don’t want to be in a relationship where all the power sits on one side. We choose to work with people who respect us for what we do, are excited to be a part of our journey, and are willing to push on our behalf. And there are plenty of those around.
Right, now I’m off to press refresh on our online banking…
Bad behaviour
Behaviour, ‘The way in which one acts or conducts oneself, especially towards others’
In other words, everything we do. The decisions we make, the way we act, the things that show people who we are.
There is so much talk about behaviour change, it’s become a buzz word. But how often do we really aim to understand behaviour, or are we really just tying to manipulate, influence and persuade someone to do something differently? Isn’t that what marketing and advertising are all about? Actually, I don’t think so.
Understanding someone’s behaviour isn’t about using it against them to hoodwink them into doing what we want them to do. It’s not about covert, subconscious ways of brainwashing people into buying what we have to sell, nor is about selling to people without them realising they are being sold to. It’s about understanding who people are and what makes them tick, so we know who we can be most relevant and meaningful for. Genuinely.
People aren’t defined by a set of demographics – I am not a a clone of every other woman in her 40s living in the London commuter belt. It is my behaviour that defines me as being me, not the facts and data about my age, where I live or what I had for dinner last night. That is equally true for an oncologist looking after people with cancer, an NHS commissioner trying to make the most out of limited resources, or a person coming to terms with a Type 2 diabetes diagnosis.
There are so many cases of behaviour impacting real-life situations in health. GPs are more likely to prescribe antibiotics just before lunch and at the end of the day, when they are weary from patients persistently demanding them. A break over lunch and they re-set their energy and resilience. People with asthma might take their inhaler diligently to start with, but gradually get complacent and feel they no longer need it, until the day they wake up finding they are struggling to breathe. I know, I am one of them, and I have given myself a stern talking to (as has the asthma nurse, who remained patient and supportive despite seeing people harming themselves like this through non-compliance every single day).
We are all people, and labels like ‘HCP’, ‘payer’ or ‘patient’ don’t help to give any understanding of who we really are. So we shouldn’t feel the need to label people like this, instead we should get to know people. Talk to them, understand what drives them, what scares them, why they do what they do. Treat them like human beings, not boxes in a survey. Then we can understand what makes them tick, what they are looking for and how we can help them with whatever it is they are looking to achieve.
Understanding people makes so much more sense than bucketing people. It’s better for them, and it’s better for us as we’re more likely to be heard. Understand people and we can talk to them in a way that suits what they need.
Behavioural insights are still largely considered to be unnecessary – not a core part of what we need to do. Why on earth not? The upfront investment can reap rewards and make everything else more efficient and effective, with proven ROI. Maybe people prefer to keep doing things the same old way, crossing their fingers that they’ll get something different and more effective out of the other end.
If we want communications to be more effective, and genuinely make a difference, we should stop thinking about how to convince and persuade, and instead start thinking about how we can listen and understand. It’s a win-win.








Christmas is only one day of the year, and we were keen to do something more long-lasting than a typical Christmas donation. Ilford Sunday drop-in caught our eye, and we’re delighted to be able to support them to expand the wonderful work they do with vulnerable and homeless people.
https://www.facebook.com/ISDFH/